Proudly part of the City Fertility Network
Proudly part of the City Fertility Network
 In Vitro Fertilisation
In Vitro FertilisationIn Vitro Fertilisation (IVF) is a fertility treatment designed to assist individuals and couples in their journey to parenthood. IVF involves fertilising an egg with sperm in a laboratory and then transferring the resulting embryo into the uterus to achieve pregnancy.
We offer access to both known and clinic-recruited sperm donors, ensuring that you have options that align with your personal preferences and family-building goals. For more details, visit our Donor Sperm page.
Rainbow Fertility has a range of donor sperm and donor eggs available, with no waitlist. Call our Fertility Advice Team on 1300 222 623 to find out more.
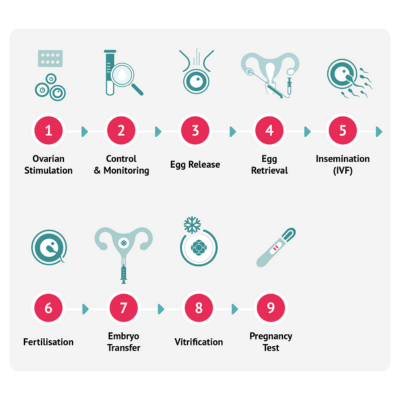
Ovarian stimulation is the first step in an IVF cycle. It involves a series of daily follicle-stimulating hormone (FSH) injections self-administered at home from Day 2 or 3 of your menstrual cycle. This medication is used to stimulate the ovaries to encourage the growth of multiple follicles containing eggs.
Your fertility specialist will closely monitor your ovarian response during the stimulation phase with ultrasounds and/or blood tests. This is important as medications may be adjusted to control the size and amount of follicles.
To assist with the final maturation of the egg and loosening of the egg from the follicle wall ready for egg collection, an injection of Human Chorionic Gonadotrophin (hCG). This is often referred to as ‘the trigger injection’.
The egg retrieval is performed 35-38 hours after ‘the trigger injection’ under ultrasound guidance and takes place while you’re lightly sedated. It is important to note that not every follicle will contain an egg, and not every egg will fertilise.
Your partner (if applicable) will be asked to produce his semen sample on the day of your procedure. If you are using frozen sperm, the sample is thawed on the day of your procedure. The sperm sample is washed and concentrated, then added to the eggs. If your specialist has recommended Intracytoplasmic Sperm Injection (ICSI), one sperm will be injected directly into each mature egg. ICSI is usually recommended for male factor infertility or previous suboptimal outcomes with standard IVF insemination.
The inseminated eggs are placed in an incubator and checked for fertilisation 16-18 hours after insemination. You will receive an update from the embryologists at this time. The normally fertilised embryos are then grown for five days. It is important to note that not every egg will fertilise, as several factors may affect the fertilisation ability of an egg and/or sperm.
Five days following egg retrieval, the embryos are assessed by the embryologists for development and quality. The best embryo is selected for transfer into the uterus using a fine plastic tube (transfer catheter). Usually only one embryo is transferred. If more than one embryo is to be transferred, this must be discussed with your clinician prior to transfer taking place. Embryo transfer is a relatively quick procedure and discomfort should be minimal.
Any remaining embryos that meet the requirements in terms of development and quality will be frozen. These frozen embryos are then stored until required for a subsequent transfer. The vast majority of frozen embryos survive the freezing process and pregnancy rates are comparable with transfer of fresh embryos.
The final stage of IVF is called the luteal phase and it’s the two weeks between the egg collection and the pregnancy test. Many people find this to be the most difficult time to endure. Whilst it’s an exciting and optimistic time of the treatment cycle, it can often be emotionally charged with expectation and anxiety. You will be encouraged to limit your activity for 24 hours after the embryo transfer, eat well, stay hydrated and keep busy while you wait for your pregnancy blood test.
Want to learn more about the IVF process? Book an appointment with one of our fertility specialists to discuss your options, or check out our in-depth IVF process guide.
We understand that every IVF journey is different. At Rainbow Fertility we tailor your quote to your individualised treatment plan, created for you by your Fertility Specialist. For a broad overview of our costs, you can visit our Treatment Costs page.
Egg retrieval
Egg retrieval is a minor procedure performed using an ultrasound-guided needle, which is carefully passed through the top of the vagina to collect eggs from the ovaries. The procedure typically takes 15–20 minutes and follows these steps:
Mild cramping, discomfort, and light vaginal spotting or bleeding are common after egg retrieval.
Following the procedure, you may begin medication to support the development of the uterine lining in preparation for embryo transfer.
Semen collection
If applicable, your partner will be asked to provide a semen sample on the day of the procedure. A private collection room is available at our clinic, or in some cases, the sample may be collected at home and brought to the clinic—this can be discussed at the start of your cycle. If you have any concerns, we encourage you to discuss them with us before your cycle begins.
Three to five days after egg retrieval, an embryo is carefully transferred into the uterus using a fine plastic tube called a catheter. The procedure is quick, typically taking just a few minutes, and is generally not uncomfortable. Many patients describe it as similar to having a pap smear.
The embryo transfer steps are:
The best-quality embryos—those with the highest chance of implantation—are prioritised for transfer. To be viable for transfer or freezing, embryos should show minimal or no fragmentation (cell breakdown) and no signs of abnormal development. If there are additional high-quality embryos, they may be frozen (vitrified) for future use.
Gender selection is not permitted in Australia unless it’s for medical reasons, such as preventing genetic conditions.
IVF stands for “In Vitro Fertilisation,” a fertility treatment where an egg is fertilised with sperm in a laboratory and then the resulting embryo is transferred into the uterus to achieve pregnancy.
Pain perception varies from person to person. For most patients, the injections taken during an IVF cycle are easy to use and relatively painless. Our experienced IVF nurses will guide you through the injection technique to help minimise any discomfort.
The egg retrieval procedure is a minor surgical procedure performed under either inhaled sedation or intravenous sedation. This means you will be either drowsy or asleep while the eggs are collected. Some patients experience mild cramping afterward, which typically resolves within a few hours. Pain relief is provided as needed.
Embryo transfer is a simple procedure that usually does not require sedation. Patients often describe it as similar to a pap smear, with only mild cramping (if any) afterward. If needed, Panadol is generally sufficient to ease any discomfort.
Potential risks and side effects associated with IVF procedures include:
IVF injections typically begin on day two or three of your period. However, the exact timing may vary based on your fertility specialist’s personalised treatment plan.